Weeks 4&5 (Ch06)
Sensory Components of Motor Control
2025-10-05
Presentation Viewing Recommendations
- This presentation is better viewed in a web browser, either on a computer or tablet. I do not recommend using mobile phones.
- Use keyboard shortcuts for navigation (e.g., arrow keys, spacebar).
- Use keyboard key “A” to pause/play audio on the current slide.
- The audio will automatically pause when you navigate to a different slide.
- Use keyboard key “S” for different viewing modes.
- If you issues with audio playback and captions, try a different web browser (e.g., Chrome, Firefox, Safari).
The PDF version of this presentation can be downloaded from the Download link at the top.
Objectives
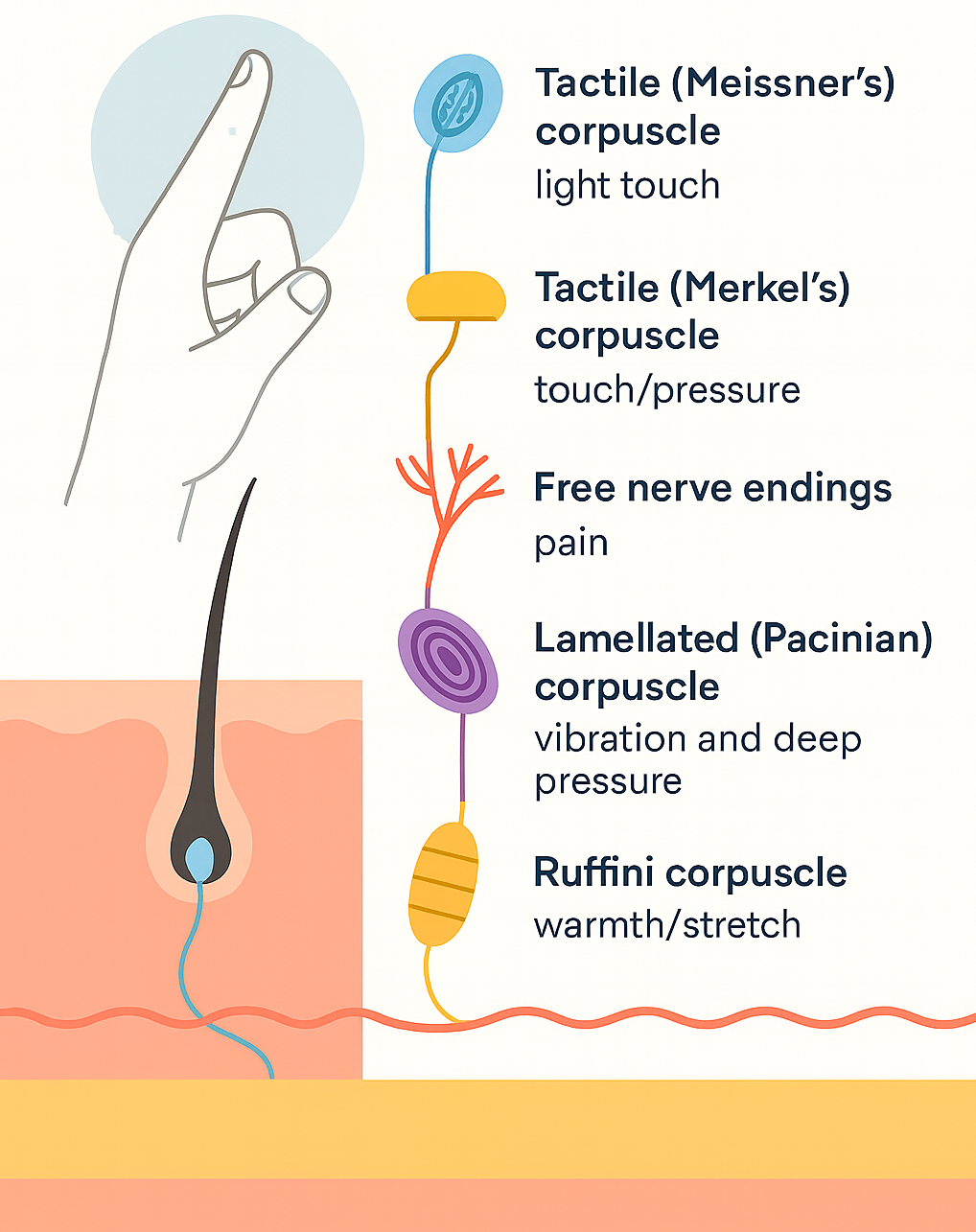
- Identify skin receptors that provide tactile information to the CNS
- Explain how tactile feedback affects accuracy, consistency, timing, and force
- Identify proprioceptors and what they signal to the CNS
- Describe classic methods to study proprioception (e.g., deafferentation, tendon vibration)
- Summarize key eye anatomy and visual pathways for motor control
- Explain methods to study vision in action (eye tracking, occlusion)
- Discuss binocular vs. monocular, central vs. peripheral vision
- Describe perception–action coupling, online visual corrections, and tau
Objectives 1-4
- Identify skin receptors that provide tactile information to the CNS
- Explain how tactile feedback affects accuracy, consistency, timing, and force
- Identify proprioceptors and what they signal to the CNS
- Describe classic methods to study proprioception (e.g., deafferentation, tendon vibration)
- You can study for the objectives using our StudyApp.
0.1 🌐 Introduction
- Sensory information is fundamental in all major theories of motor control & learning
- Roles across the action timeline:
- Pre-movement → specify parameters of action
- Online (during movement) → provide feedback for adjustments
- Post-movement → evaluate goal achievement
- Pre-movement → specify parameters of action
- Focus in this section:
- ✋ Touch (tactile system)
- 🌀 Proprioception
- 👀 Vision (fully covered in objectives 5–8) - coming soon.
- ✋ Touch (tactile system)
0.2 ✋ Touch & Motor Control: Overview
- Touch provides essential feedback for achieving action goals in daily skills
- Skin receptors (mechanoreceptors):
- Located in the dermis
- Densest in fingertips → support precision
- Signal pressure, stretch, vibration, temperature, pain
- Located in the dermis
- Critical for:
- Object manipulation (e.g., grasping, typing, playing piano)
- Interactions with people/environment (e.g., walking, sports)
- Object manipulation (e.g., grasping, typing, playing piano)
0.3 Neural Basis of Touch (at a glance)
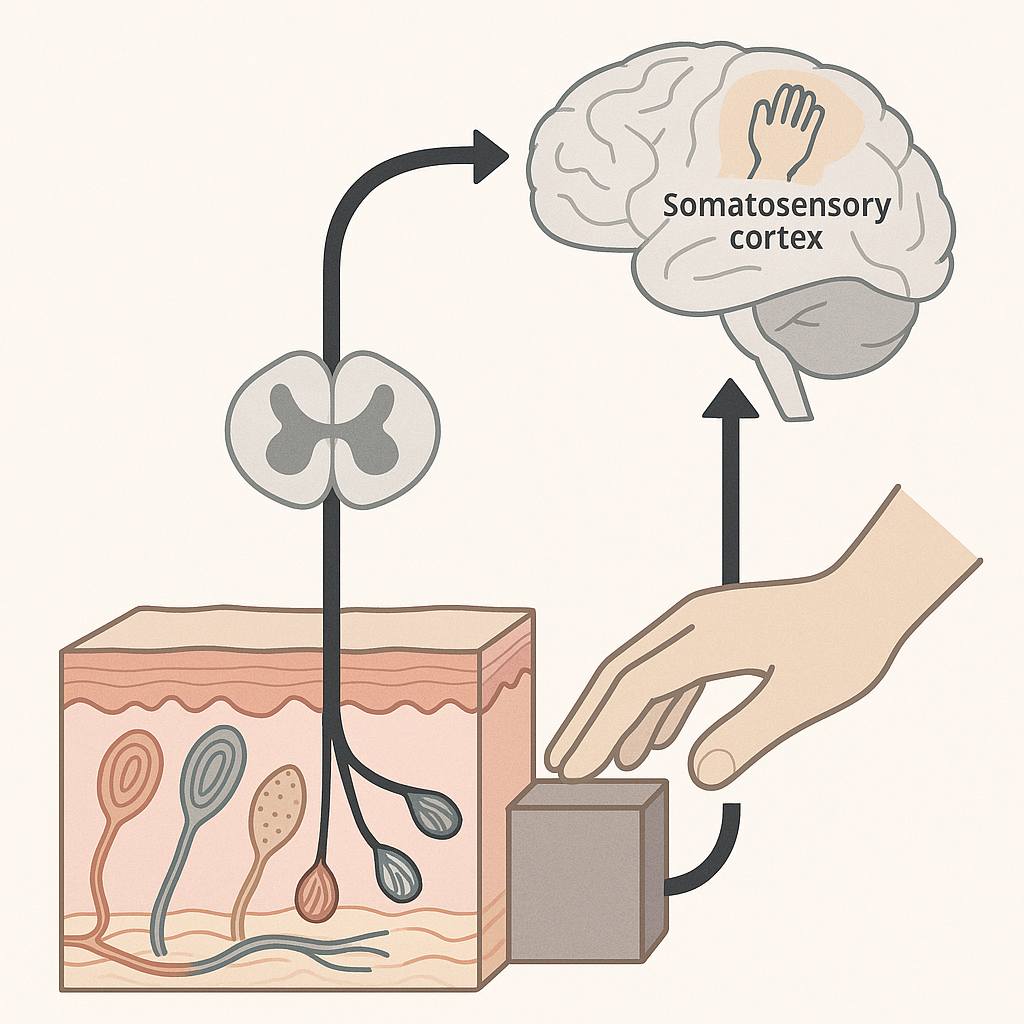
- Mechanoreceptors in the skin transduce deformation into neural signals
- Tactile information travels via ascending somatosensory pathways
- Signals reach the somatosensory cortex, integrating with motor areas
- This feedback enables action planning, adjustment, and control
0.4 🖐️ Roles of Tactile Information in Motor Control
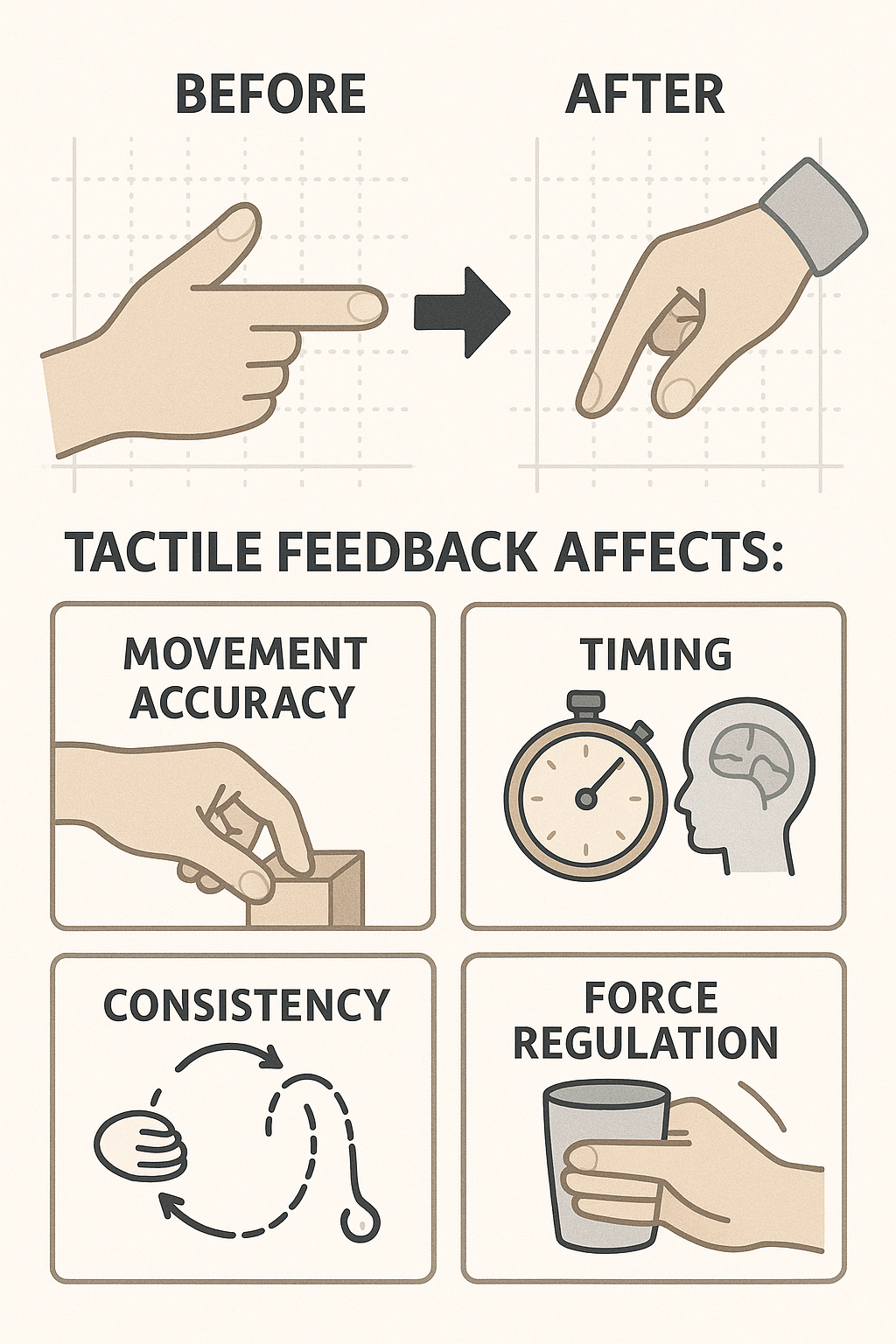
- Experimental approach: Compare motor performance before and after anesthetizing fingertips
- Tactile (cutaneous) feedback affects:
- ✅ Movement accuracy — especially in pointing, grasping, and fine motor skills
- 🔁 Consistency — reduces variability in repeated movements
- ⏱️ Timing — crucial for rhythmic actions and phase transitions (e.g., tapping, circle drawing)
- 🧠 Force regulation — helps scale grip force and adjust mid-movement (e.g., lifting a cup)
- ✅ Movement accuracy — especially in pointing, grasping, and fine motor skills
Tactile input supports precision, rhythm, and adaptability in everyday and skilled movements.
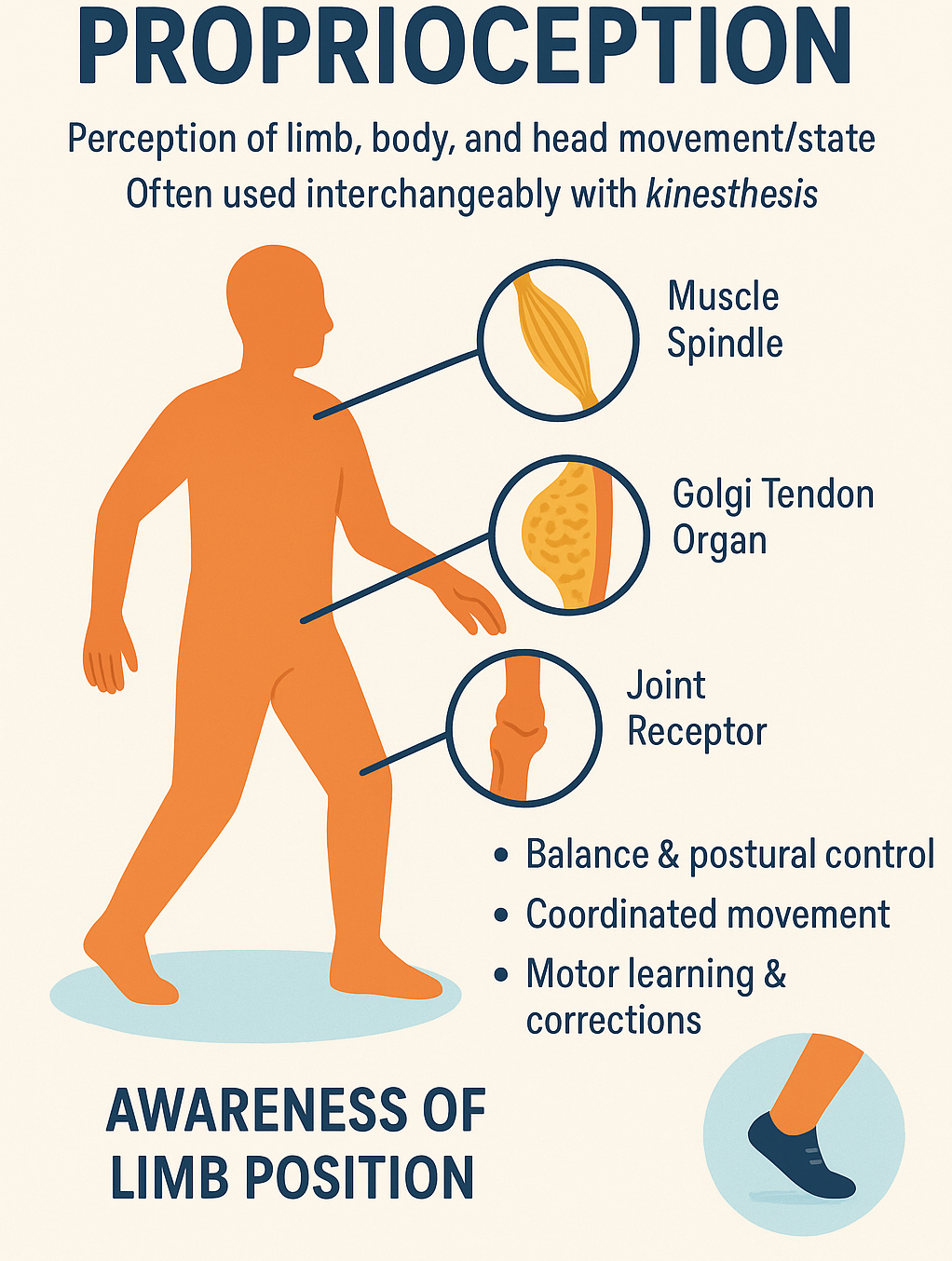
0.5 Proprioception: Definition
Proprioception is the body’s ability to sense the position, movement, and force of limbs, trunk, and head — even without visual input.
- Sometimes used interchangeably with kinesthesis
- Involves feedback from muscle spindles, Golgi tendon organs, and joint receptors
- Critical for:
- Balance and postural control
- Coordinated movement
- Motor learning and corrections
📌 Essential for executing movements like walking, reaching, and grasping — even in the dark!
0.6 🧩 Neural Basis of Proprioception
- Proprioceptors are sensory neurons located in:
- Muscles, tendons, ligaments, and joints
- Muscles, tendons, ligaments, and joints
- They provide continuous feedback about limb position, movement, and force
- Three primary classes:
- Muscle spindles → detect changes in muscle length & velocity
- Golgi tendon organs (GTOs) → detect muscle tension/force
- Joint receptors → detect joint angle & movement at extremes of motion
- Muscle spindles → detect changes in muscle length & velocity
- Proprioceptive signals travel via the dorsal column-medial lemniscal pathway to the somatosensory cortex
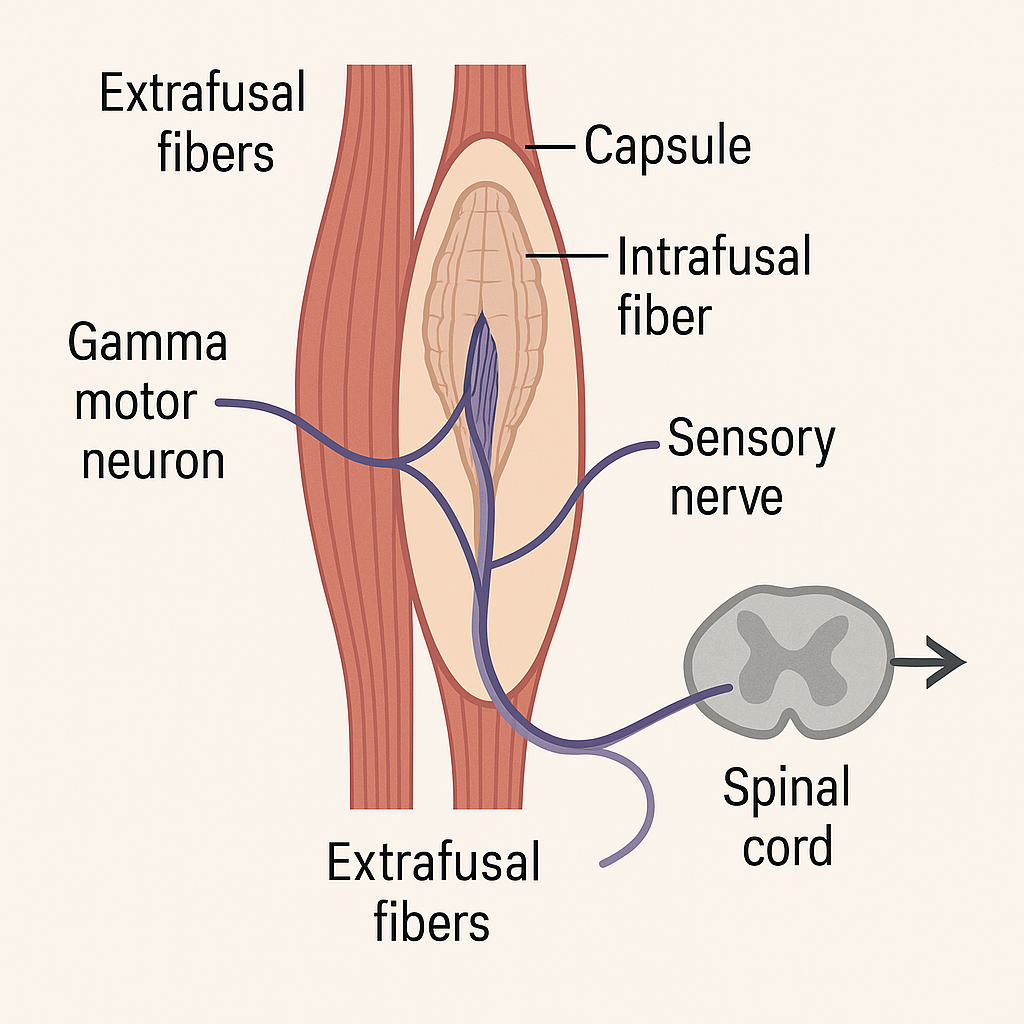
0.7 💪 Muscle Spindles (1)
- Encapsulated intrafusal fibers located within most skeletal muscles
- Arranged in parallel with force-generating extrafusal fibers
- Sensory endings (type Ia afferents) wrap around the central region → detect muscle length & velocity
- Innervated by gamma motor neurons (fusimotor system) → maintain spindle sensitivity during contraction
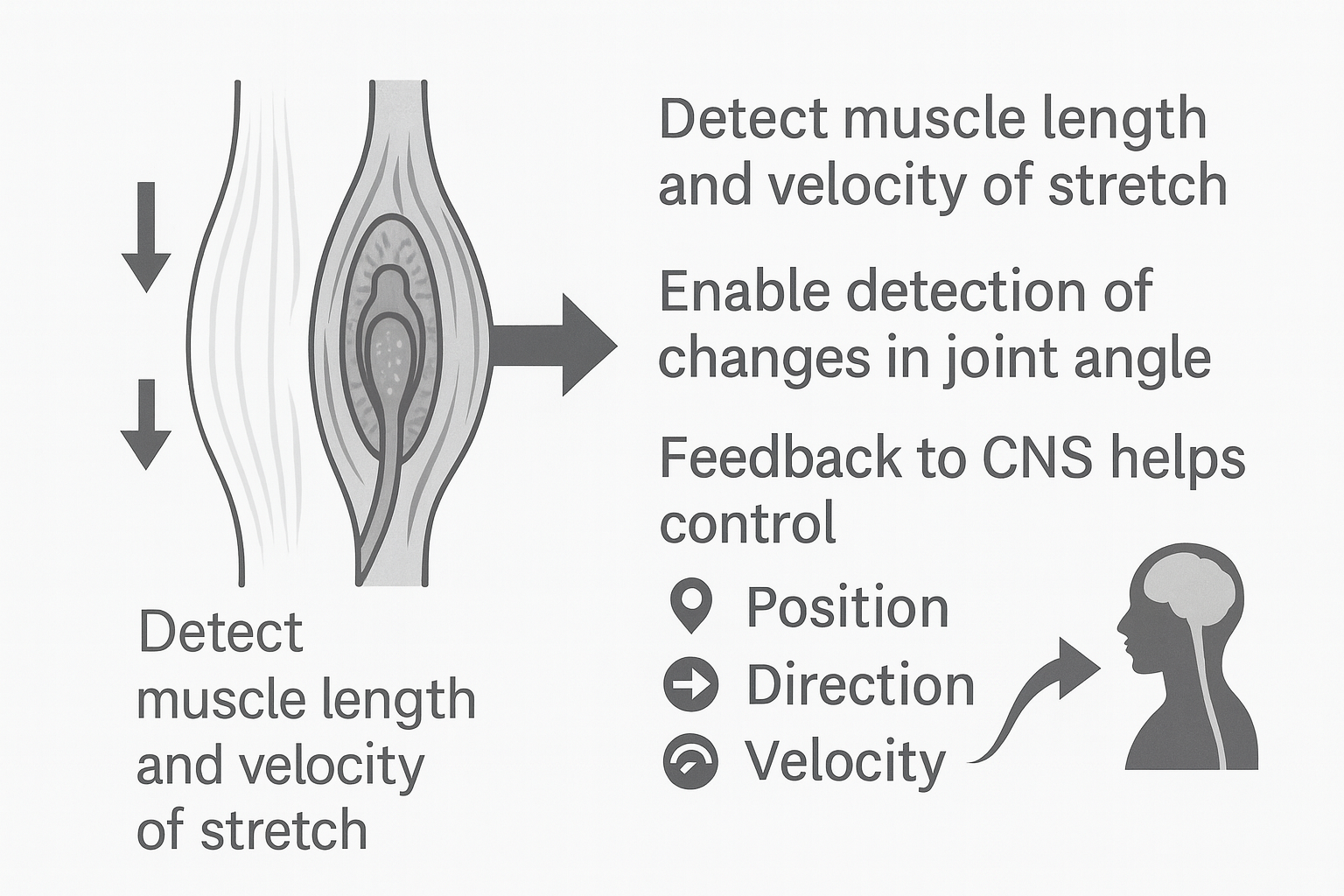
0.8 🌀 Muscle Spindles (2)
- Detect muscle length and velocity of stretch
- Provide sensory basis for joint angle changes
- Continuous feedback to CNS supports control of:
- Position (limb placement in space)
- Direction (movement trajectory)
- Velocity (speed of movement)
- Position (limb placement in space)
- Critical for both movement correction and planning
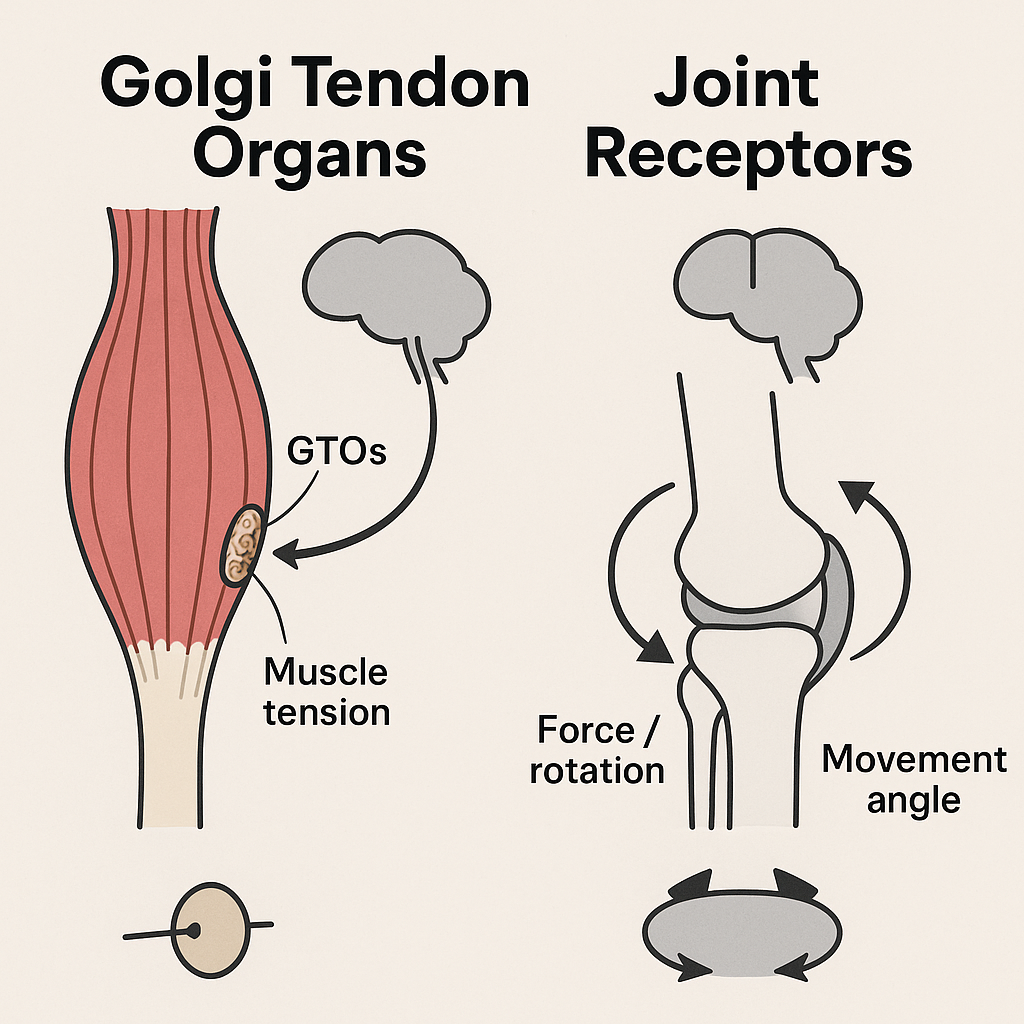
0.9 ⚖️ Golgi Tendon Organs & Joint Receptors
- Golgi Tendon Organs (GTOs):
- Located near tendon insertions in skeletal muscle
- Detect muscle tension / force (not length)
- Provide inhibitory feedback to prevent excessive force
- Located near tendon insertions in skeletal muscle
- Joint Receptors:
- Found in joint capsules and ligaments
- Detect force, rotation, and movement angle
- Especially sensitive at end ranges of motion
- Include Ruffini endings, Pacinian corpuscles, and Golgi-like receptors
- Found in joint capsules and ligaments
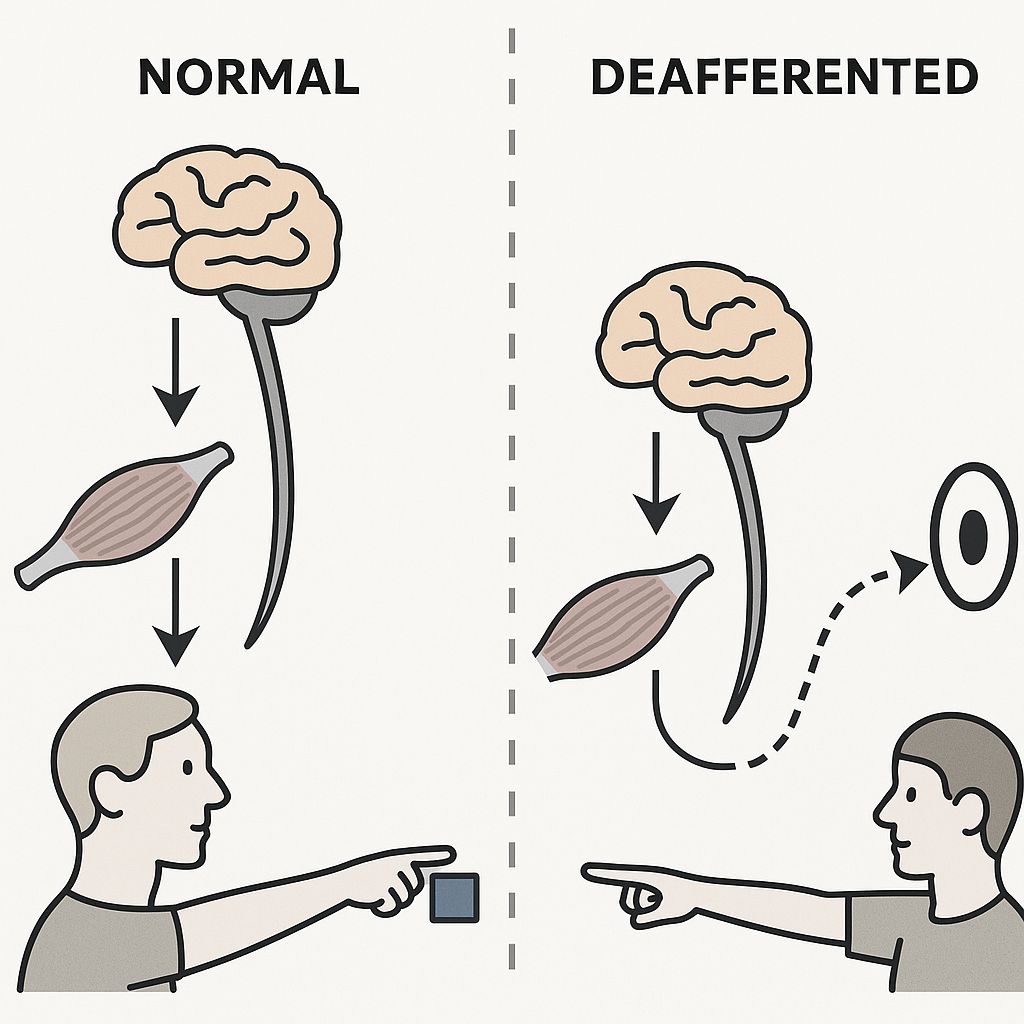
0.10 🧪 Investigating Proprioception: Deafferentation
- Surgical deafferentation
- Afferent pathways severed or removed (animal studies, rare clinical cases)
- Used to study how loss of proprioceptive input alters movement control
- Afferent pathways severed or removed (animal studies, rare clinical cases)
- Sensory neuropathy (peripheral neuropathy)
- Loss of large myelinated afferents → profound proprioceptive deficits
- Pain & temperature sensation often preserved
- Movements show spatial errors, poor smoothness, and lack of coordination
- Loss of large myelinated afferents → profound proprioceptive deficits
- Research example: Blouin et al. (1993) cited in Magill & Anderson (2017)
- Compared deafferented patient vs. healthy controls in a pointing task
- With vision: performance nearly normal
- Without vision: patient consistently undershot targets
- Compared deafferented patient vs. healthy controls in a pointing task
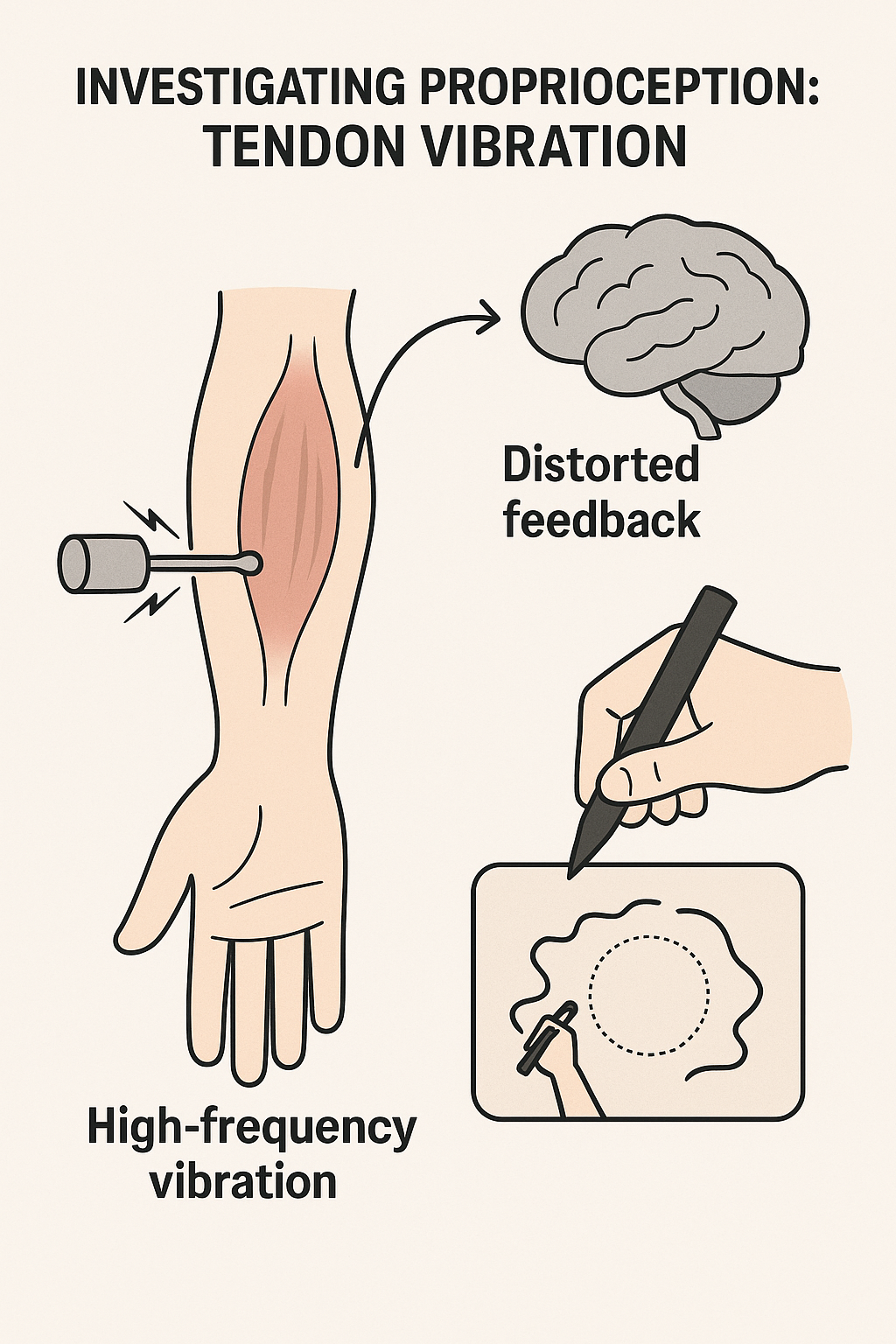
0.11 🎵 Investigating Proprioception: Tendon Vibration
Method: Apply high-frequency vibration to the tendon of an agonist muscle
Effect: Distorts proprioceptive feedback → creates illusory lengthening of the muscle
Unlike deafferentation, feedback is altered (not removed)
Used to study proprioceptive contribution to movement control & coordination
Research example: Verschueren et al. (1999) cited in Magill & Anderson (2017)
- Vibrating biceps/anterior deltoid altered arm trajectory in circle drawing
- Showed disrupted spatial accuracy and inter-limb coordination
- Vibrating biceps/anterior deltoid altered arm trajectory in circle drawing
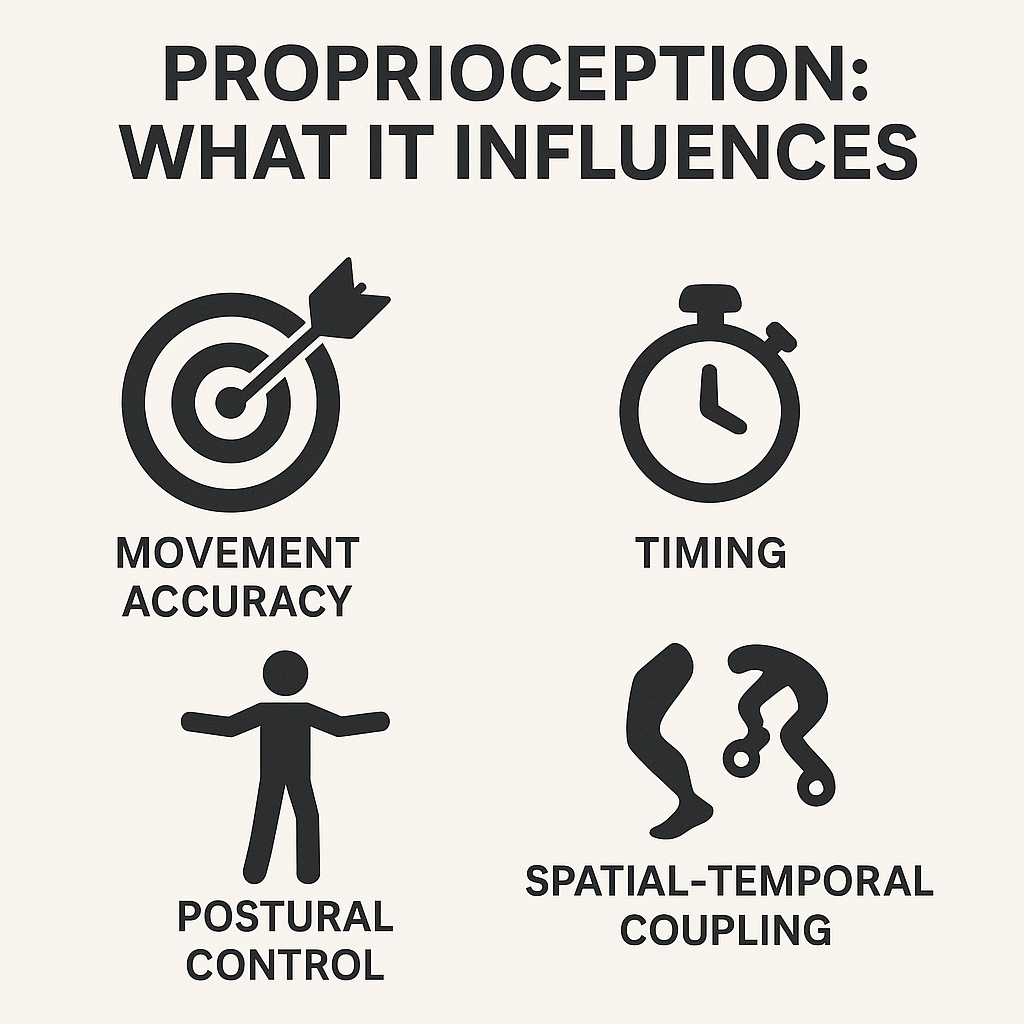
0.12 ⚙️ Proprioception: What It Influences
- Movement accuracy
- Critical for spatial & temporal precision
- Errors increase without proprioceptive feedback
- Critical for spatial & temporal precision
- Timing
- Influences onset of motor commands
- Coordinates sequencing of limb actions
- Influences onset of motor commands
- Coordination
- Supports segmental coupling within and across limbs
- Ensures smooth multi-joint movement patterns
- Supports segmental coupling within and across limbs
Major takeaways: Objectives 1-4
- Both provide critical feedback for motor control
- Touch: important for object manipulation and fine motor skills
- Proprioception: essential for movement accuracy, timing, coordination, postural control
- Loss or distortion of either impairs motor performance
- CNS integrates tactile and proprioceptive info for smooth, coordinated actions
- Both are vital for skilled movement execution
- Understanding their roles aids in rehabilitation and skill training
- Next: Vision & Motor Control
Slides for objectives 5-8 are coming soon!
Objectives 5-8
- Summarize key eye anatomy and visual pathways for motor control
- Explain methods to study vision in action (eye tracking, occlusion)
- Discuss binocular vs. monocular, central vs. peripheral vision
- Describe perception–action coupling, online visual corrections, and tau
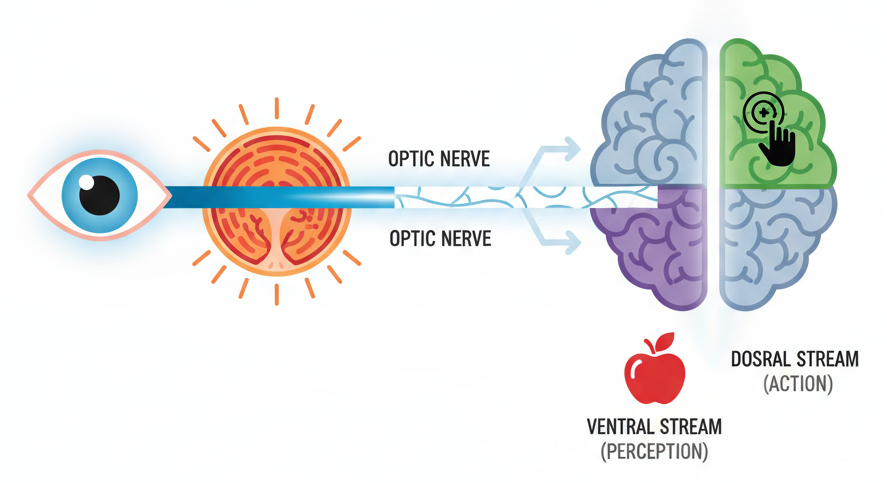
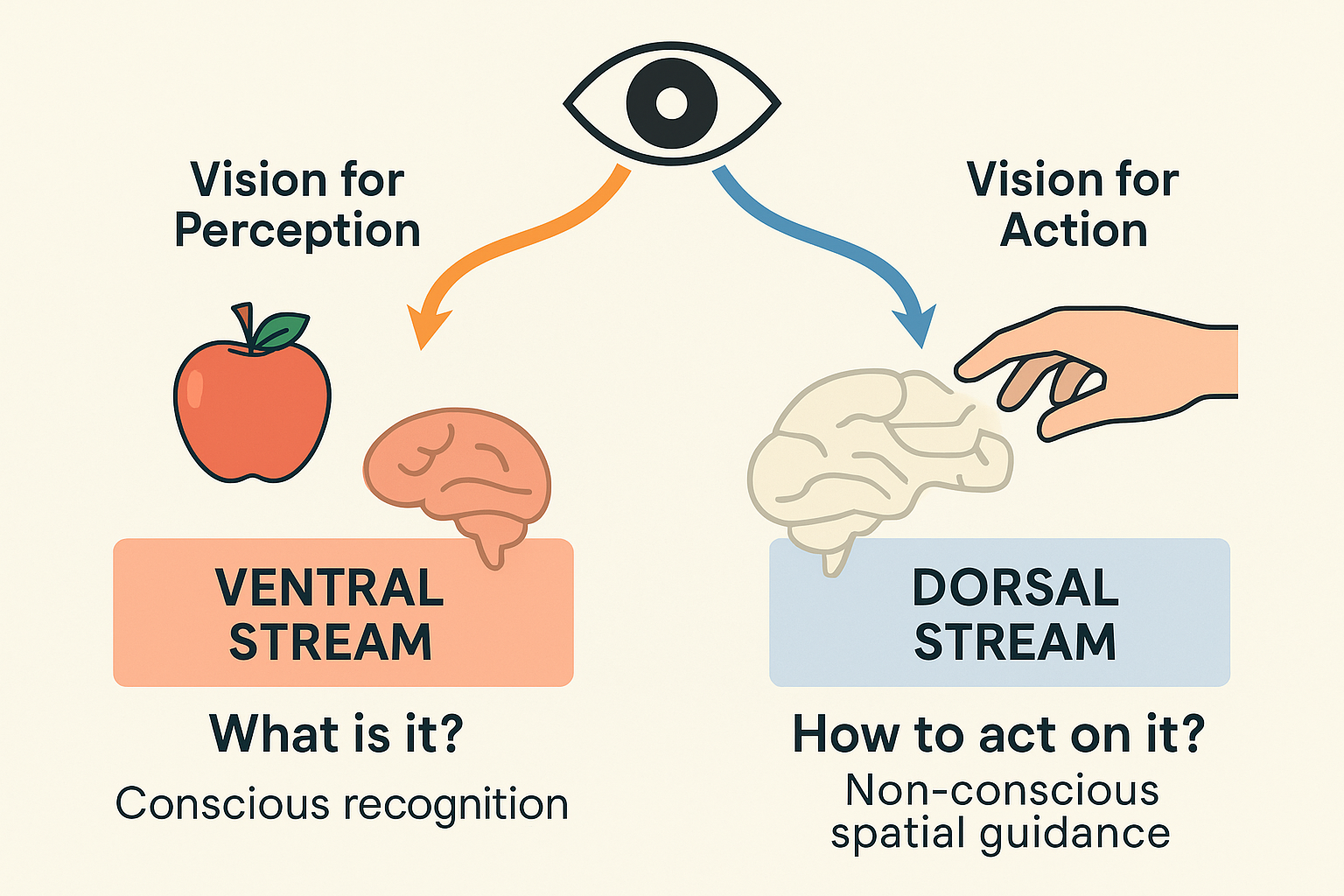
0.13 👁️ Vision: Neurophysiology (Overview)
- Eye → Retina → Optic nerve → Subcortical & Cortical pathways
- Retina: photoreceptors (rods & cones) transduce light → neural signals
- Parallel processing streams:
- Ventral (“vision-for-perception”) → object identification (form, color, detail)
- Dorsal (“vision-for-action”) → spatial guidance & movement control
- Ventral (“vision-for-perception”) → object identification (form, color, detail)
- Integration with motor areas enables targeting, tracking, and corrections
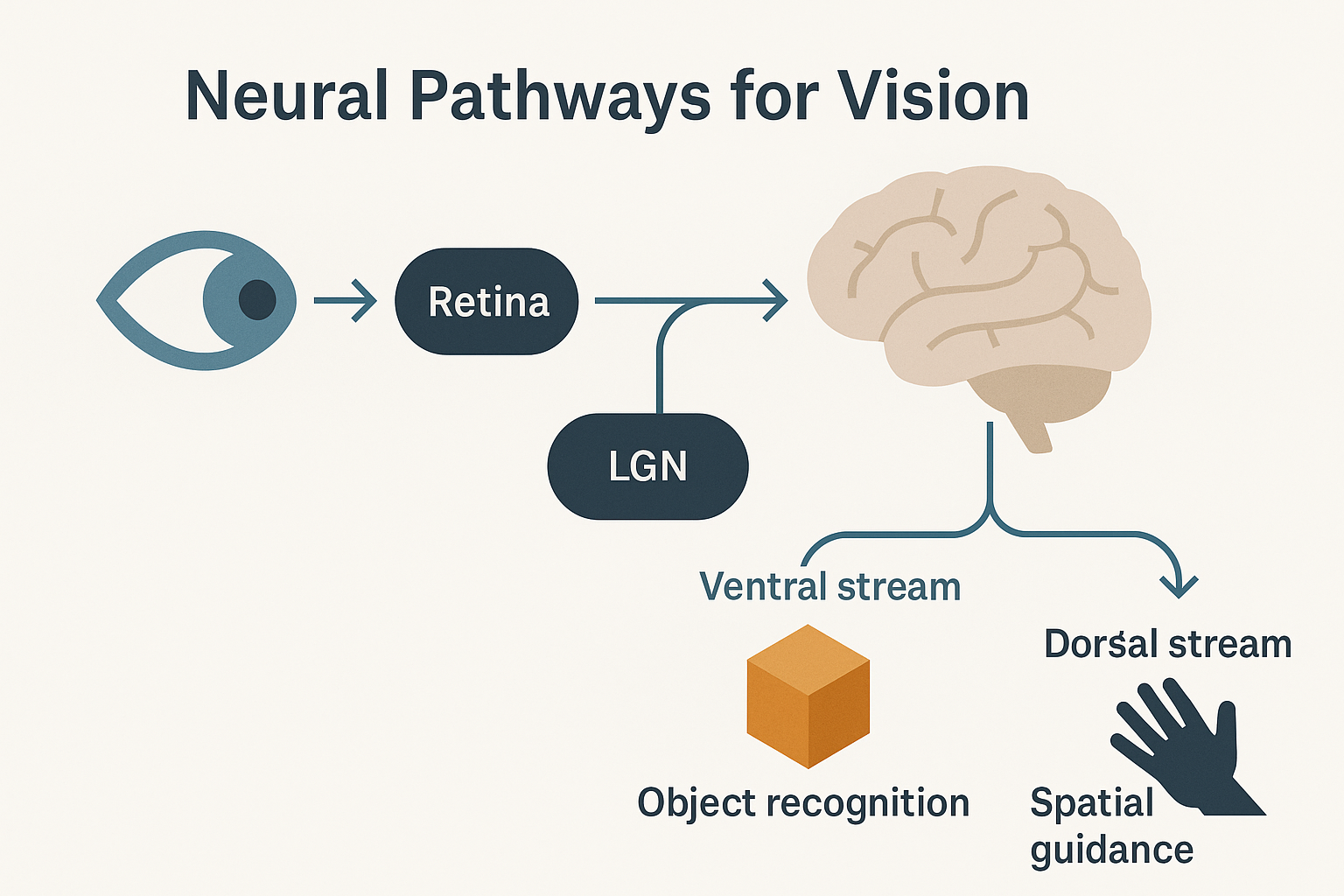
0.14 👁️ Neural Pathways for Vision (Overview)
- Light enters the retina, photoreceptors transduce light into neural signals
- Signals travel via the optic nerve and cross at the optic chiasm
- Relayed to the lateral geniculate nucleus (LGN) of the thalamus
- Projected to the primary visual cortex in the occipital lobe
- From the cortex, information diverges into two parallel streams:
- Ventral stream (vision-for-perception): object recognition and identification
- Dorsal stream (vision-for-action): spatial guidance and movement control
- Ventral stream (vision-for-perception): object recognition and identification
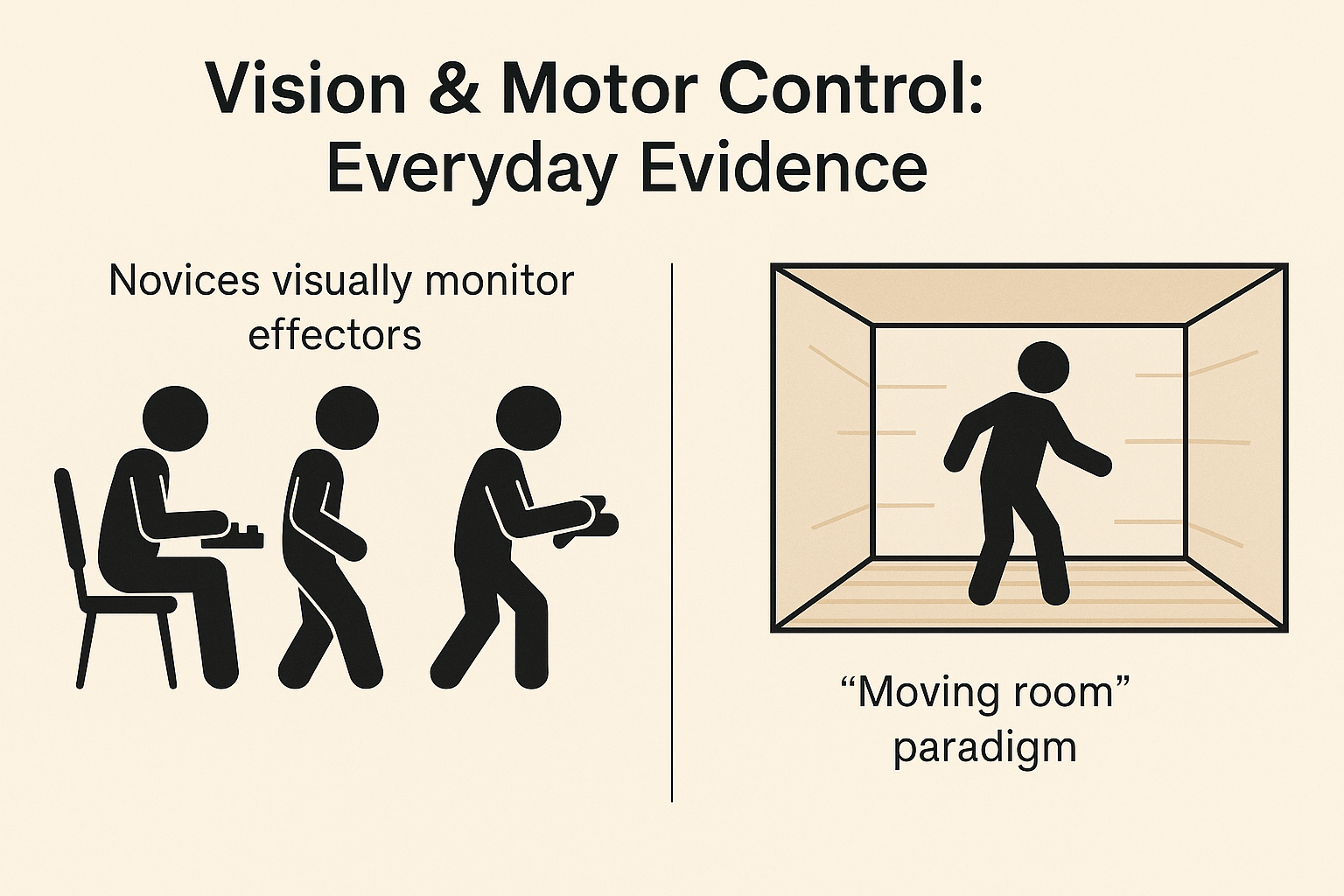
0.15 👀 Vision & Motor Control: Everyday Evidence
- Novices rely on vision to monitor effectors
- Typists looking at their fingers
- Dancers watching their feet
- New drivers visually scanning every control
- Typists looking at their fingers
- With skill development, reliance on vision decreases as tactile and proprioceptive feedback increase
- Classic “moving room” paradigm (Lee & Aronson)
- Visual cues can override proprioceptive and vestibular information
- Demonstrates visual dominance in postural control
- Visual cues can override proprioceptive and vestibular information
- Everyday life: vision provides continuous reference for balance, posture, and spatial orientation
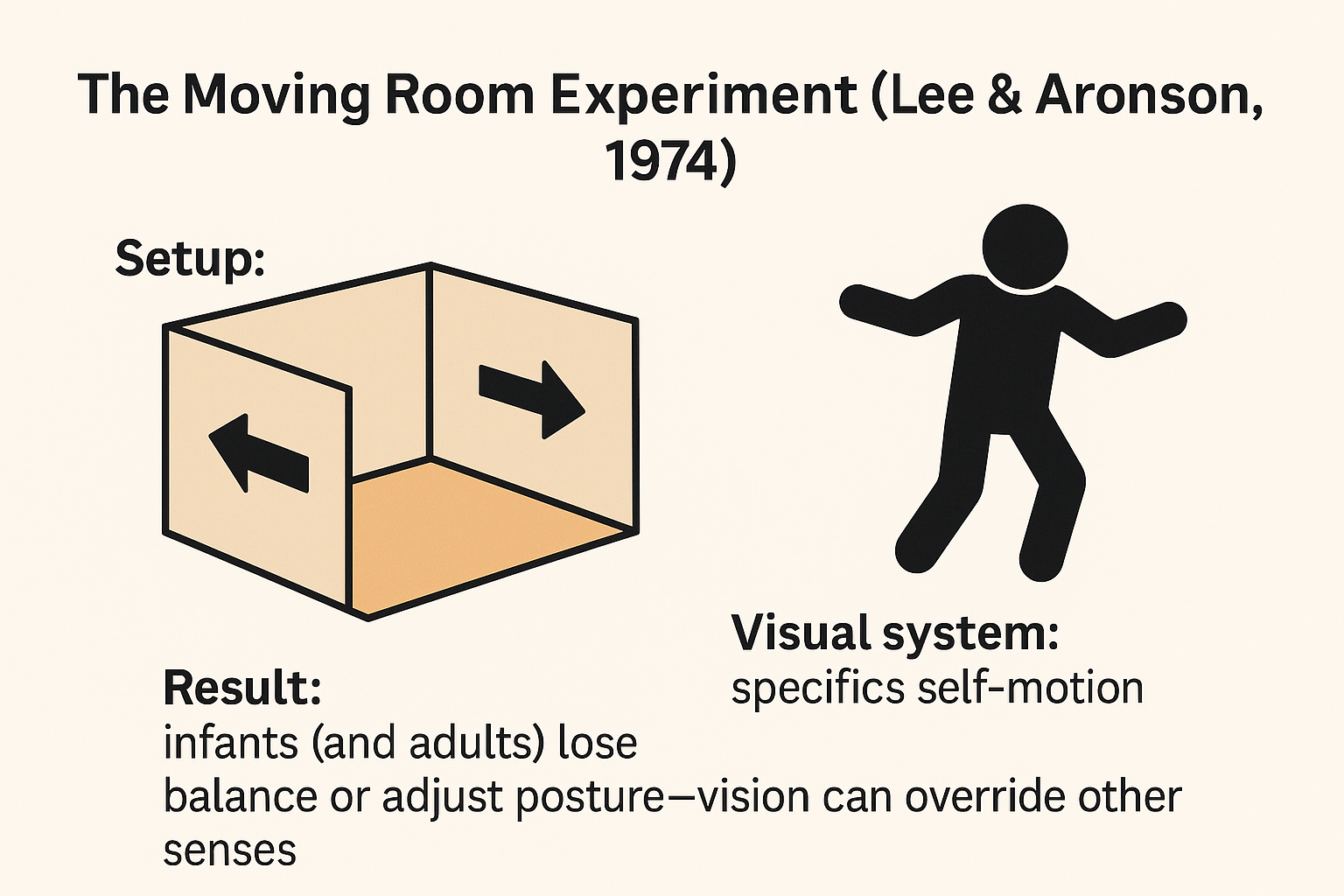
0.16 🏠 The Moving Room Experiment (Lee & Aronson, 1974 cited in Magill & Anderson (2017))
- Setup:
- Walls and ceiling of the room move back and forth
- Floor remains completely stationary
- Walls and ceiling of the room move back and forth
- Conflict of sensory information:
- Visual system: signals self-motion
- Vestibular & somatosensory systems: signal no movement
- Visual system: signals self-motion
- Findings:
- Infants and adults sway, stumble, or lose balance
- Demonstrates visual dominance—vision can override other senses in postural control
- Infants and adults sway, stumble, or lose balance
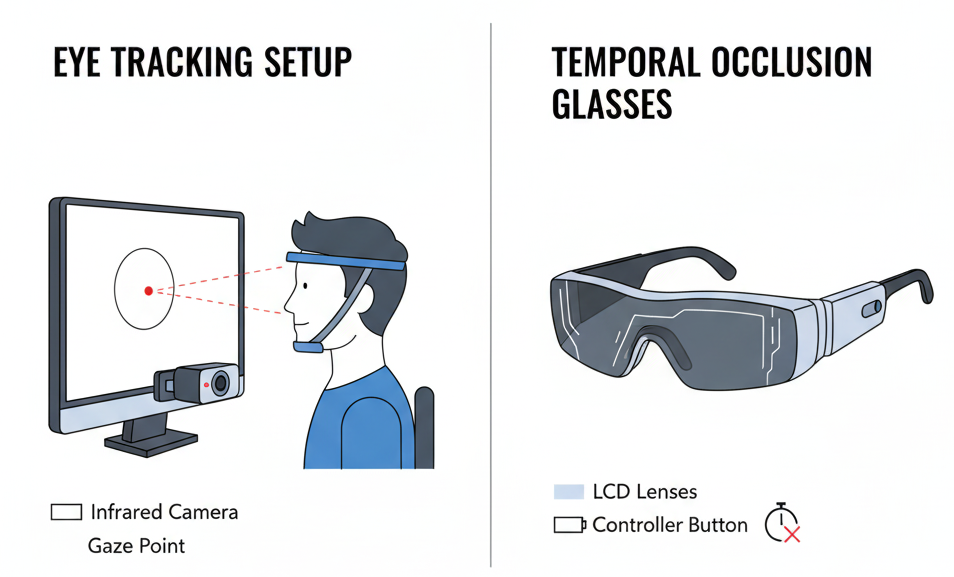
0.17 🎥 Studying Vision in Action (1): Methods
- Eye-movement recording
- Tracks where the eyes are looking and for how long
- Identifies point of gaze (foveal vision) during skill performance
- Tracks where the eyes are looking and for how long
- Temporal occlusion techniques
- Stop video at different time points to test when critical information is detected
- Use of liquid-crystal spectacles (PLATO glasses) to control viewing windows in real time
- Stop video at different time points to test when critical information is detected
- Provide insights into how vision is used for anticipation, decision-making, and movement control
0.18 🎥 Studying Vision in Action (2): Methods
- Event occlusion techniques
- Mask selected features of the performer (e.g., arm, racquet) or the environment in video or film sequences
- Prevents the observer from seeing certain critical cues
- Mask selected features of the performer (e.g., arm, racquet) or the environment in video or film sequences
- Purpose
- Identifies which specific visual information performers rely on
- Determines when this information is used during performance
- Identifies which specific visual information performers rely on
- Provides insight into visual strategies for anticipation, decision-making, and motor skill execution
Refer to figure 6.8 in the textbook Magill & Anderson (2017) for an example of event occlusion in a tennis serve.
0.19 👁️ Role of Vision in Motor Control: Key Aspects
- Monocular vs. Binocular vision
- Binocular vision improves depth perception and movement accuracy
- Monocular vision reduces efficiency, especially at greater distances
- Binocular vision improves depth perception and movement accuracy
- Central vs. Peripheral vision
- Central (foveal) vision detects fine detail and object features
- Peripheral vision provides spatial context, guiding locomotion and posture
- Central (foveal) vision detects fine detail and object features
- Two visual systems
- Ventral stream (vision-for-perception): recognition, description
- Dorsal stream (vision-for-action): spatial guidance, movement control
- Ventral stream (vision-for-perception): recognition, description
- Perception–action coupling
- Visual information is tightly linked with motor execution
- Time course of corrections
- Vision-based adjustments typically require ~100–160 ms
- Time-to-contact (tau)
- Optical variable tau specifies when to initiate or adjust action
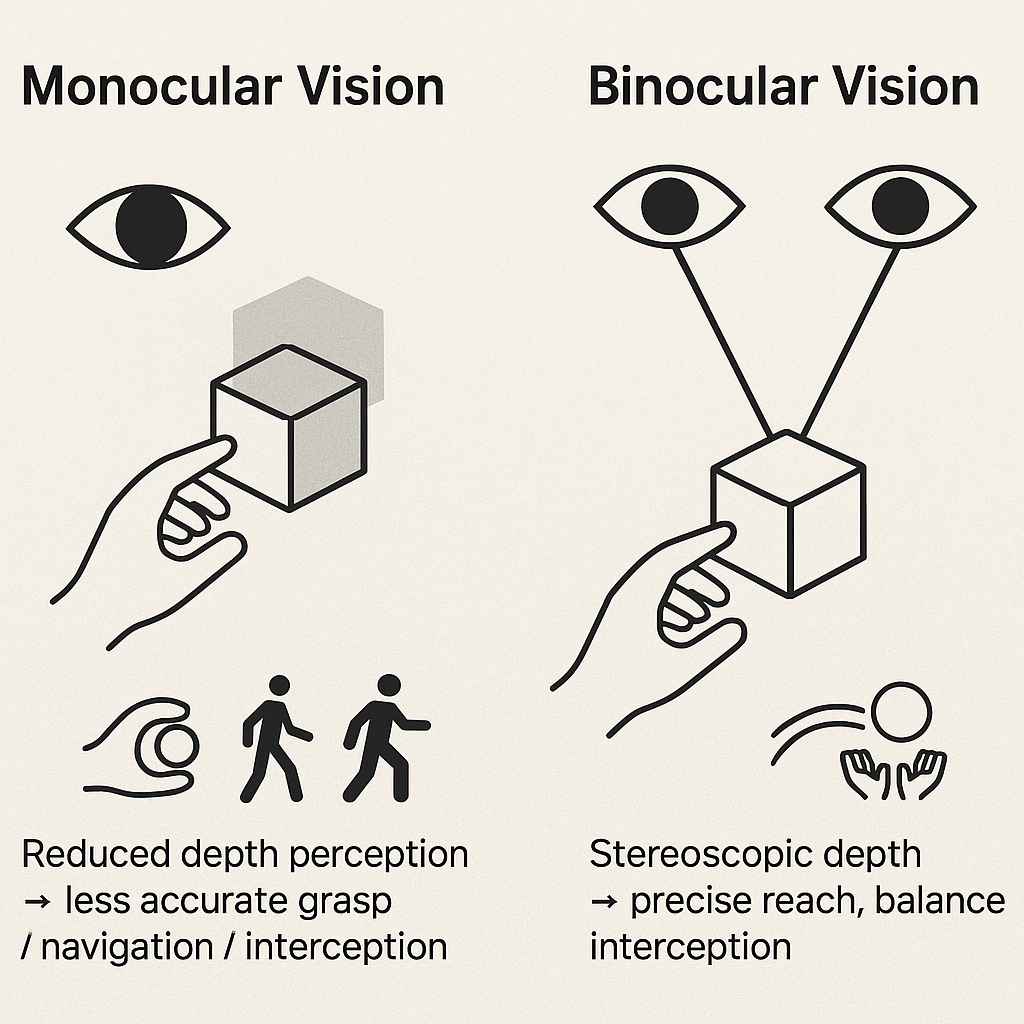
0.20 👀 Monocular vs. Binocular Vision
- Binocular vision
- Provides depth perception and 3D spatial accuracy
- Critical for:
- Reaching and grasping objects
- Walking through cluttered or uneven environments
- Intercepting moving objects (e.g., catching, hitting)
- Reaching and grasping objects
- Provides depth perception and 3D spatial accuracy
- Monocular vision
- Can support performance but with reduced accuracy and efficiency
- Leads to underestimation of distance and object size
- Errors more pronounced as distance to target increases
- Can support performance but with reduced accuracy and efficiency
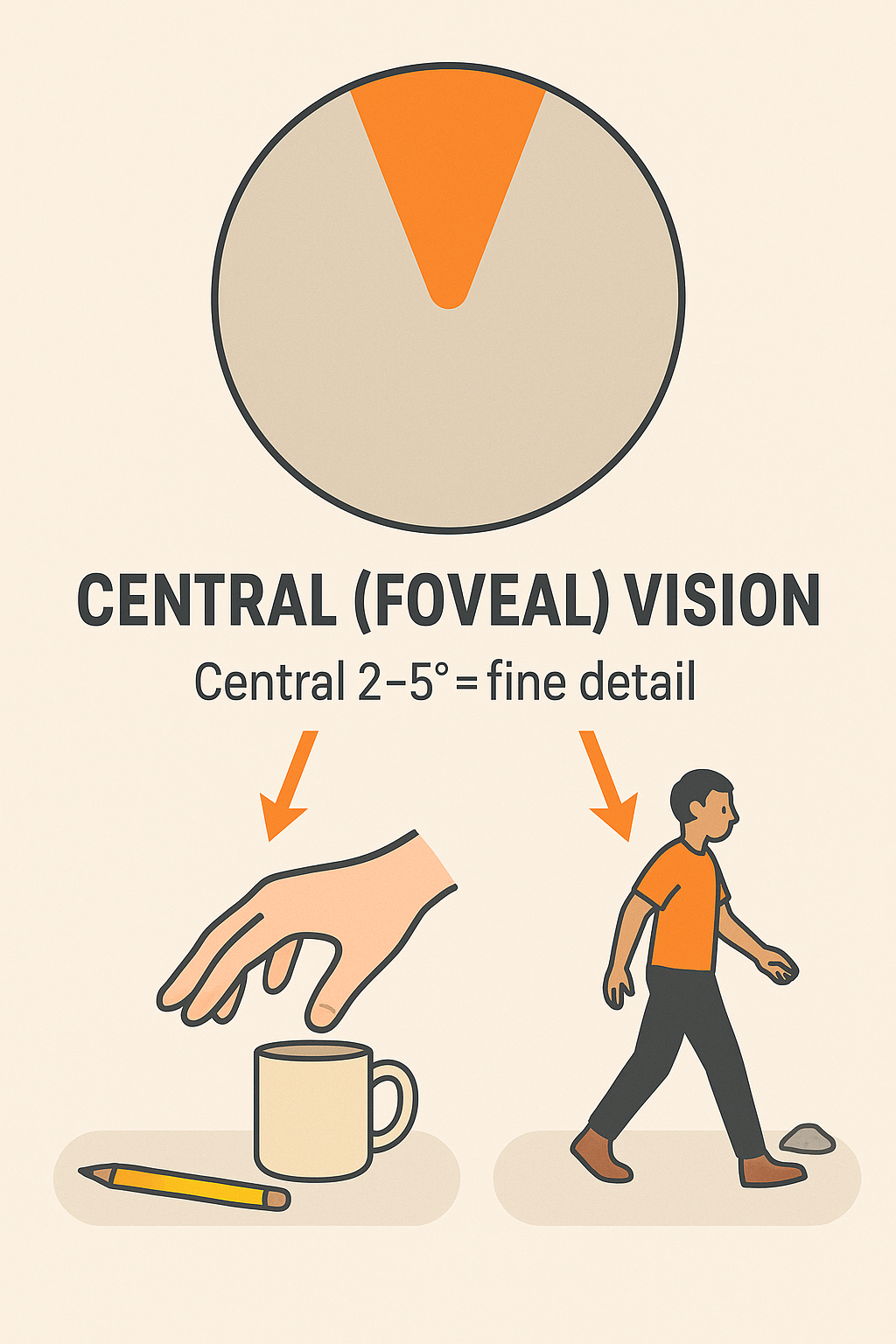
0.21 🎯 Central (Foveal) Vision
- Covers the central ~2–5° of the visual field (foveal vision)
- Responsible for detecting fine detail and specific features
- Provides critical information to support action goals:
- Reaching & grasping
- Detects object regulatory conditions (size, shape, orientation)
- Guides grip formation and movement trajectory
- Detects object regulatory conditions (size, shape, orientation)
- Locomotion
- Supplies precise path and obstacle details
- Supports accurate foot placement and navigation
- Supplies precise path and obstacle details
- Reaching & grasping
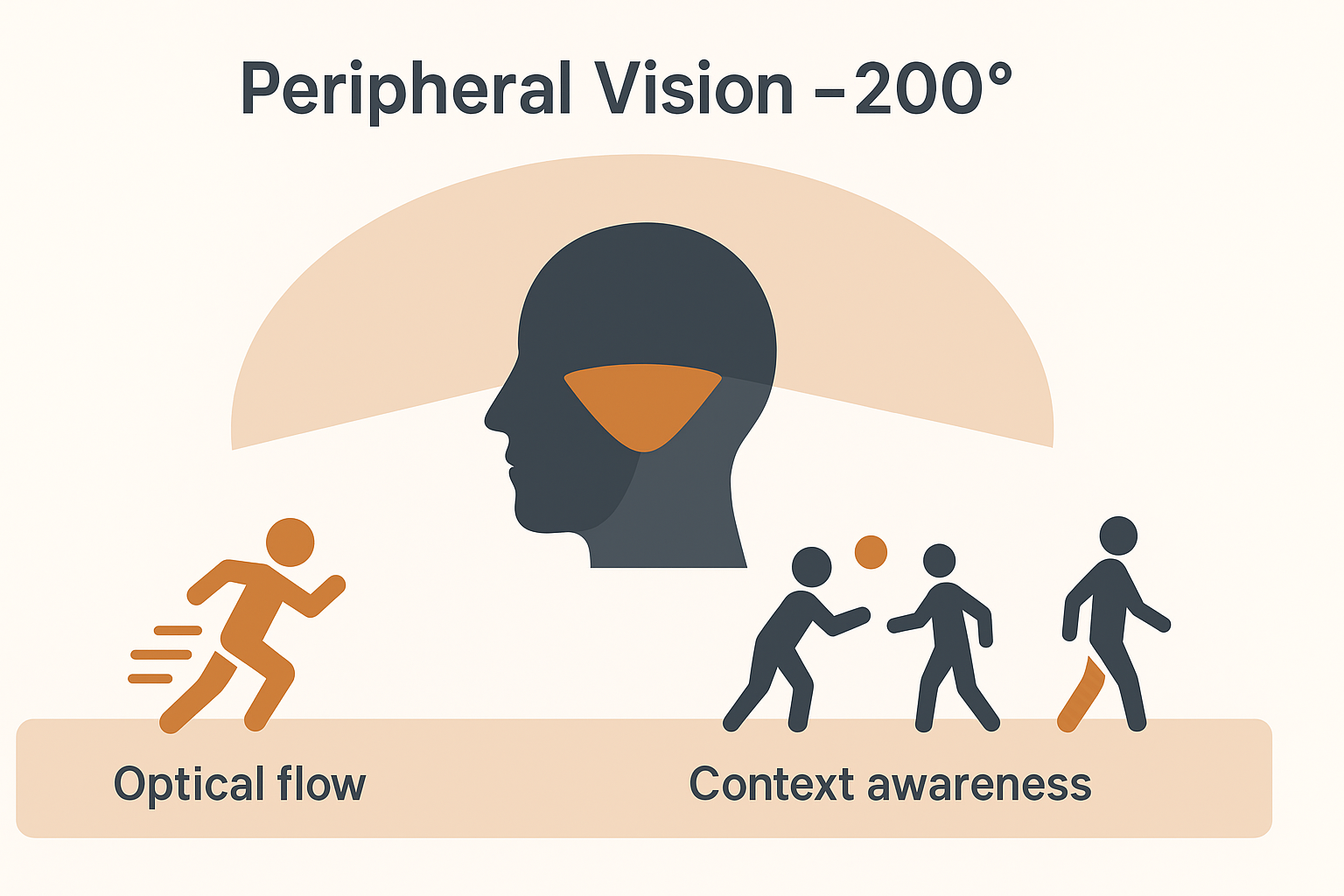
0.22 👁️ Peripheral Vision
- Extends across ~200° of the visual field
- Provides contextual information beyond the central 2–5°
- Contributes to perception of own limb movement during actions
- Essential for optical flow:
- Pattern of motion across the retina created by self-movement
- Guides posture, locomotion, and orientation in space
- Pattern of motion across the retina created by self-movement
- Supports navigation through the environment and coordination with moving objects or people
0.23 👓 Two Visual Systems
- Vision-for-Perception (Ventral stream)
- Pathway: visual cortex → temporal lobe
- Fine analysis of visual scene: form, color, features
- Supports object recognition and description
- Information is typically conscious
- Pathway: visual cortex → temporal lobe
- Vision-for-Action (Dorsal stream)
- Pathway: visual cortex → posterior parietal lobe
- Provides spatial characteristics of objects and environment
- Guides movement planning and online control
- Processing often occurs non-consciously
- Pathway: visual cortex → posterior parietal lobe
- Streams operate in parallel → perception and action are supported simultaneously
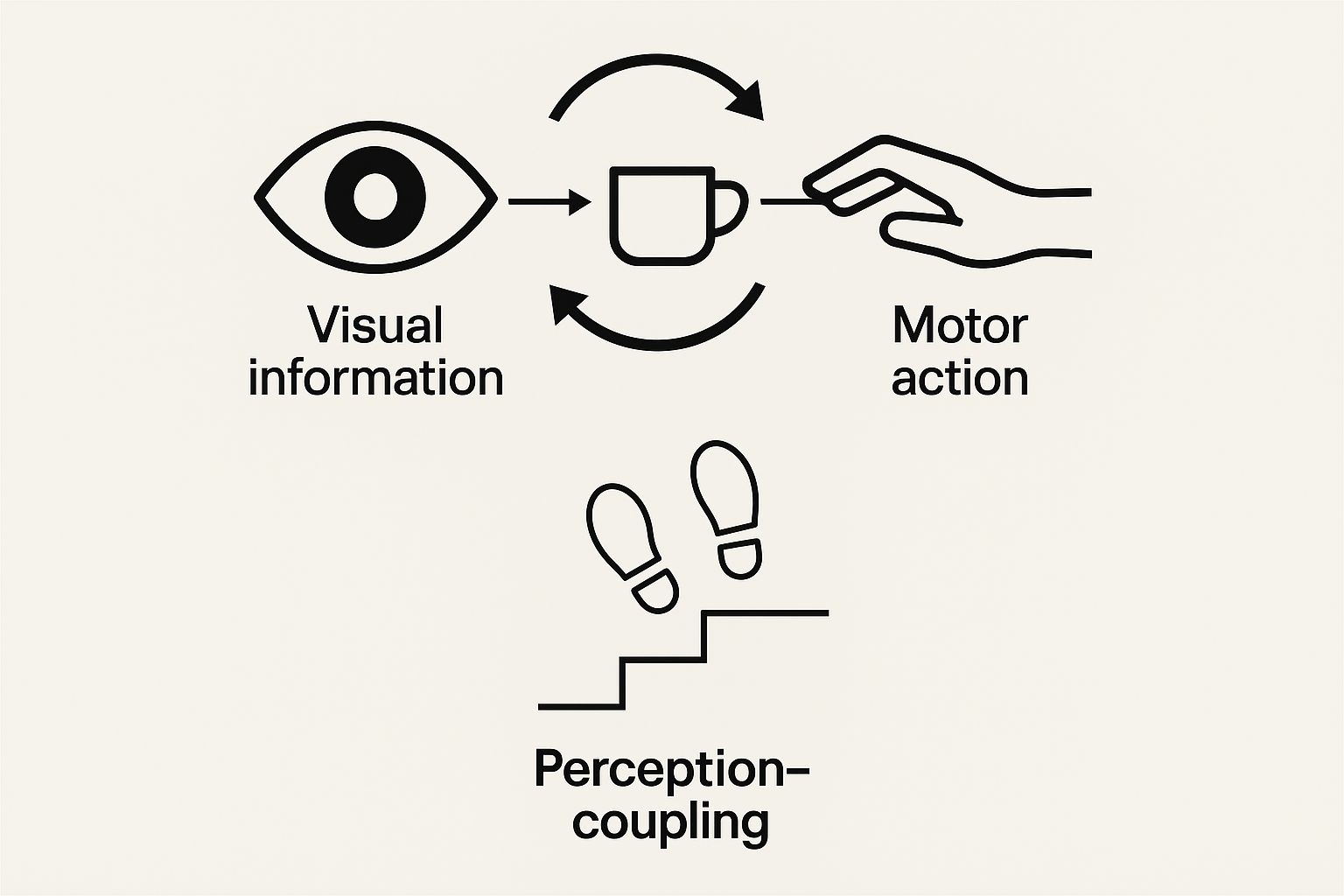
0.24 🔗 Perception–Action Coupling
- Perceptual information and motor actions are tightly connected
- Visual perception continuously informs movement parameters
- Eye–hand coordination as a classic example:
- Spatial and temporal features of gaze align with limb kinematics
- Point of gaze typically arrives at the target before the hand
- Spatial and temporal features of gaze align with limb kinematics
- Coupling ensures movements are adjusted online to match environmental demands
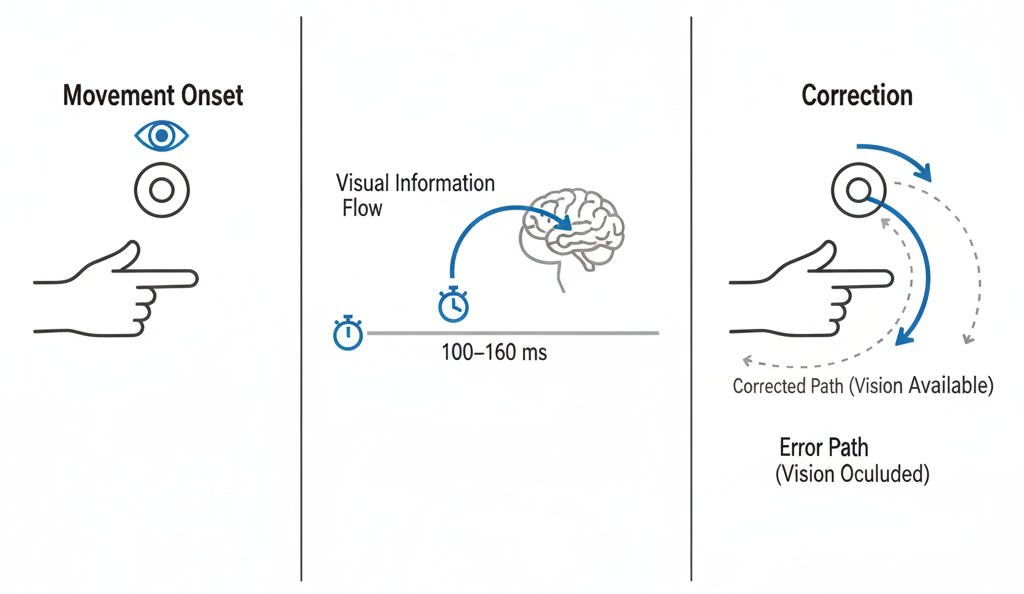
0.25 ⏱️ Online Visual Corrections: Time Required
- Experimental approach
- Compare rapid aiming when target is visible vs. occluded after movement onset
- If vision is available, corrections can be made mid-flight
- If vision is removed, errors increase
- Compare rapid aiming when target is visible vs. occluded after movement onset
- Time window for corrections
- Visual feedback requires ~100–160 ms to process
- Corrections possible only if movement duration allows this window
- Visual feedback requires ~100–160 ms to process
- Implications
- Fast, ballistic movements often too brief for corrections
- Slower or sustained movements benefit from visual feedback adjustments
- Fast, ballistic movements often too brief for corrections
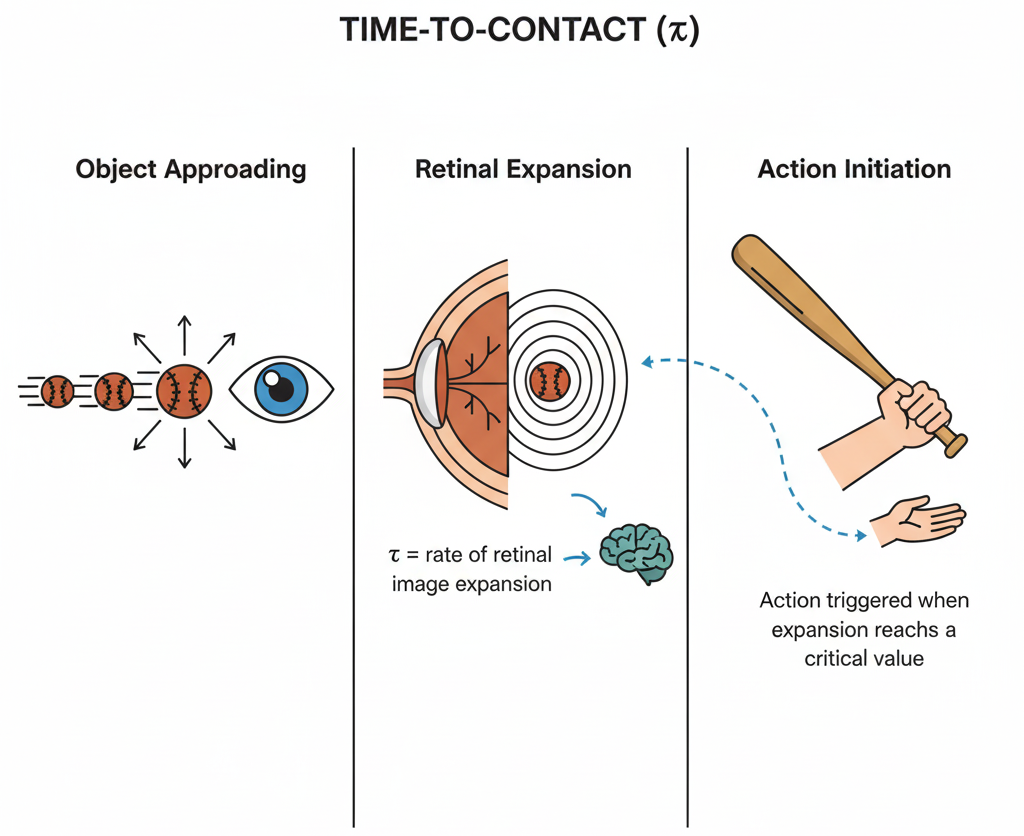
0.26 ⏳ Time-to-Contact (τ)
- In interception and avoidance tasks, vision specifies when to initiate action
- Optical variable tau (τ):
- Derived from the rate of expansion of an object’s image on the retina
- Provides a direct estimate of time remaining until contact
- Derived from the rate of expansion of an object’s image on the retina
- At a critical expansion rate, action is automatically triggered (non-conscious)
- Allows precise movement initiation in dynamic contexts:
- Catching or hitting moving objects
- Avoiding oncoming obstacles
- Timing steps or braking when approaching surfaces or vehicles
- Catching or hitting moving objects
✅ Major Takeaways (Ch. 06)
Touch & Proprioception (Obj. 1–4)
- ✋ Tactile feedback supports accuracy, timing, consistency, and force regulation; anesthetizing fingertips degrades performance
- 🧩 Proprioceptors (muscle spindles, GTOs, joint receptors) signal length/velocity, tension, and joint position → essential for posture, coordination, and movement correction
- 🧪 Classic methods: deafferentation (loss of afferents) and tendon vibration (illusory lengthening) reveal proprioception’s role
- 🏥 Training & rehab: task-specific practice that enriches cutaneous + proprioceptive feedback improves skill and recovery
- 🧠 Pathways: Retina → LGN → V1 → ventral (perception) and dorsal (action) streams running in parallel
Vision & Motor Control (Obj. 5–8)
- 🔭 Monocular vs. binocular: binocular depth boosts 3D tasks (reach–grasp, navigation, interception)
- 🎯 Central vs. peripheral: central = fine detail/regulatory conditions; peripheral = context, limb motion, optical flow for posture/locomotion
- 🔗 Perception–action coupling: gaze timing aligns with limb kinematics; eyes arrive before the hand
- ⏱️ Online corrections: vision-driven adjustments emerge in ~100–160 ms—fast moves rely more on feedforward
- ⌛ Time-to-contact (τ): retinal image expansion rate specifies when to initiate action, often non-consciously
So what?
- The CNS integrates touch, proprioception, and vision to plan, guide, and evaluate movement
- Effective instruction/rehab leverages the right sensory cues for the task (detail vs. context; depth; feedback timing)
- Designing practice that matches sensory demands (visibility, textures, loads, speeds) accelerates learning and recovery
0.27 💡 Points to the Practitioner
🔍 Assess Sensory Deficits - Movement problems may stem from touch, proprioception, or vision deficits - Examples: - Poor balance post-stroke may indicate proprioceptive loss, not just weakness - Gait instability could reflect somatosensory rather than motor deficits
👁️ Use Vision as Compensatory Strategy - Clients rely on vision to substitute for compromised sensory systems - PT Applications: - Mirror feedback for posture training - Visual targets for reaching exercises - Gait training with floor markers/visual cues
🎯 Optimize Visual Attention - Direct central vision appropriately for motor tasks - Clinical Examples: - “Look at the target” during functional reaching - Eye-hand coordination in ADL retraining - Visual tracking exercises for sports return
⏰ Consider Processing Time - Corrections require sufficient time for sensory-motor integration - Rehabilitation Applications: - Slow movement speeds for neurological clients - Adequate reaction time in fall prevention training - Progressive speed increases in sports rehab
0.28 🏥 Additional Clinical Considerations
🩺 Special Populations - Diabetic neuropathy → tactile feedback loss affecting balance/gait - Joint replacement → altered proprioception requiring retraining - Parkinson’s disease → reduced proprioceptive processing - Multiple sclerosis → variable sensory deficits affecting motor control
🎯 Advanced Training Techniques - Closed-eye balance training → force proprioceptive reliance - Dual-task training → divided attention challenges - Sensory integration exercises → combine multiple sensory inputs - Perturbation training → unexpected challenges to reactive systems
🧠 Cognitive & Environmental Factors - Age-related changes → slower processing, reduced acuity - Medication effects → sedation, dizziness impacting integration - Cognitive load → reduce complexity for motor learning - Attention deficits → impact sensory-motor coupling
🌍 Environmental Modifications - Lighting optimization → improve visual input quality - Surface texture → enhance tactile/proprioceptive feedback - Visual contrast → aid object detection and depth perception - Noise reduction → minimize sensory distractions
References

Download | Ovande Furtado Jr., Ph.D. | CSUN | KIN Department | KIN479 Motor Control | Course Site